Breast/chest feeding is the most natural thing in the world. However, for some it can be challenging, yet somehow it is so easy for others. Lift your top, latch your baby in a relaxed position, done! Once you decide you want to try breast/chest feeding, so many questions suddenly arise. Our experienced midwife and babywearing consultantKatrin Ritter knows this situation only too well. That's why we've collected our most frequently asked questions from new parents and had Katrin provide you with her expert advice in the answers below.
Breastfeeding tips: The 10 most frequently asked questions about breast/chest feeding:
1. Baby falls asleep while breast/chest feeding - is that bad?
The smaller your baby is, the more likely they are to fall asleep while breast/chest feeding. A full tummy makes babies tired and fall asleep naturally. Some babies empty the breast/chest in a few minutes and fall asleep contentedly. If your newborn sleeps a lot, barely wakes up to nurse and falls asleep after just a few swallows, he or she may not be getting enough fluid and nutrients needed. In addition, your milk production will not start properly if your little one does not drink enough. If this is the case, it can help to undress your baby a little before breast/chest feeding, to change the nappy in between or to alternate sides more often to keep them awake to feed. A lot of light, massaging the feet or gently stroking/tickling the back can also keep your baby from falling asleep. Please contact your health visitor or midwife with any concerns or questions.

2. Baby spits up after breast/chest feeding, should I be worried?
If your baby spits up milk during or after breast/chest feeding, this is called reflux. This is normal because the sphincter of the stomach is still weak. As your baby gets older, he or she will spit up less and less. At about 12 months, your baby should have outgrown this reflex. You can find out how to counteract spitting up after breast/chest feeding here.
Always listen to your gut feeling. Of course, spitting up can also be caused by something pathological. If you are unsure, please ask your midwife or paediatrician.
3. Why do I get my period even though I am breast/chest feeding?
Due to hormonal changes and high prolactin levels, it is common for menstrual cycles to stop during breast/chest feeding. Every person’s body is different and depending on how much you breast/chest feed, your period can return anywhere between just a few weeks to many months after giving birth. Often women don't get their periods back until their baby is largely eating solid food and they breast/chest feed less. One thing is clear: You can still breast/chest feed when your period starts. It is possible that the amount of milk will be slightly reduced when your bleeding starts, and baby might be a little fussy, but this usually regulates itself very quickly.
4. How long can you breast/chest feed with a nipple shield?
The motto is: as much as necessary but as little as possible. Most lactation consultants and midwives prefer to use a nipple shield for a few weeks or less and only recommend its use if other measures have not helped and, of course, only after baby’s latch has been properly assessed. The longer a nipple shield is used, the harder it usually is to stop. If you need more support or have further questions, please ask your midwife or breastfeeding support team.
5. Baby bites when breast/chest feeding - what should you do?
Many breast/chest feeding mothers and breast/chest feeding experts recommend taking your baby off the breast/chest if they bite and calmly tell your little one that you don't want him or her to bite as it hurts. Being bitten in the nipple can hurt a lot and is a shock at first. However, try not to jerk your baby away from your breast and cry out. This could lead you to injure your nipple even more or scaring baby initiating a ‘nursing strike’. Stay calm and try to loosen your child's jaw by pushing your little finger into the corner of their mouth. Most of the time, the jaw will loosen by itself. As biting is often caused by distraction, it can help to go to a dark and/or quiet place to breast/chest feed and keep an eye out for signs of baby getting bored or coming to the end of a feed. Shortly after you have released your baby from the breast/chest, feeding can be resumed and if you like you can praise your baby for latching on well.
6. How long and often should a newborn breast/chest feed?
A newborn should be breast/chest fed frequently to quickly make up for the weight lost during the first days on this planet and, of course, to stimulate milk production. A baby can eat about 8 to 12 times per 24 hours. On average, babies drink about 15-20 minutes per side, some longer, some shorter. Particularly in the course of cluster feeding (periods of long, continuous breast/chest feeding), breast/chest feeding can sometimes extend to an hour or more. Keep an eye on baby and their feeding to ensure they are drinking or just suckling to settle. Carrying them, with or without a carrier, bathing or cuddling skin-to-skin can also help to calm your baby during periods when they are unsettled.

7. Baby sweats when breast/chest feeding - why?
Holding your baby skin-to-skin to drink can make you feel warm quickly, and can be tiring for baby as the process of drinking, sucking and digesting the milk is a lot of work and effort for them. You may notice that newborns sweat after feeding, whether they have been breast/chest fed or bottle-fed. In this case, it is a good idea to pause the feeding session and help them cool down before continuing with the meal. Despite possible sweating, skin to skin contact has a positive effect on the secure bond between mother and child, your baby is aware of your smell and heartbeat and feels safe and secure.
8. How to dry up breast milk supply?
The time will come when you and your child are ready to wean. Unless necessary for medical reasons it is advisable to take some time for this and not just go “cold turkey”. If baby is under 12 months old they will need either breast/chest or formula milk as a replacement. The La Leche League and NHS website has some helpful information to support you.

9. Is breast/chest feeding OK after a caesarean section?
Yes, absolutely! Try and maximise skin to skin time with your baby as soon as possible after birth. In usual circumstances a midwife can help you lie skin-to-skin while you are still in the operating theatre or recovery room. Skin-to-skin contact releases the hormone oxytocin, which stimulates milk production. After a caesarean section, it is advisable to stay on your back with the baby lying on top of you. It makes sense to put your baby on the breast/chest as soon as possible after birth so that he or she can crawl to the breast/chest on their own.
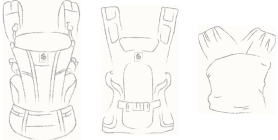
10. Breast/chest feeding and carrying - how can I breast/chest feed in a baby carrier?
One of the biggest advantages of a baby carrier is that it encourages the flow of milk through physical closeness, making breast/chest feeding easier. And you can even breast/chest feed in your carrier when you are out and about. We show you exactly how this works and what you should pay attention to in various videos on our Instagram channel @ergobabyuk.
We hope this blog has answered all your questions? If not, check out our blog search function to see if you can find more on breast/chest feeding.
We will be back with a second part blog with breast/chest feeding tips soon!